The rising incidence of Alzheimer’s Disease (AD) in our aging population has spurred a global effort to understand its underlying causes. Among the pressing questions that many families face is, “Is Alzheimer’s hereditary?” Unpacking this question requires a deep dive into the current body of research, which paints a multifaceted picture of the disease. This article explores the genetic elements associated with AD and how they may play a role in an individual’s susceptibility.
The Foundations of Alzheimer’s: A Brief Overview
Alzheimer’s Disease is a progressive neurodegenerative disorder characterized by memory loss, cognitive decline, and the inability to perform everyday tasks. It’s most commonly diagnosed in individuals over 65, but early-onset Alzheimer’s can appear in people as young as 40. The exact cause of AD remains a mystery, but both environmental and genetic factors are believed to play a role.
The Role of Genetics in Alzheimer’s Risk
Scientists have identified a number of genes that may increase the risk of developing AD. These genes can be broadly categorized into deterministic genes and risk genes.
Deterministic Genes
These are genes that guarantee the development of a disease if they are present. In the context of Alzheimer’s, mutations in these genes typically result in early-onset familial Alzheimer’s Disease (FAD). Individuals with these mutations almost always develop FAD before the age of 65.
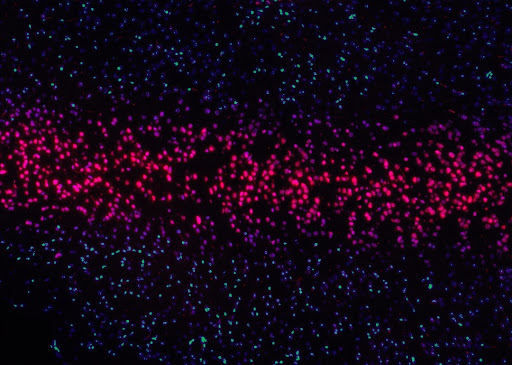
Three major genes fall under this category: APP (Amyloid precursor protein), PSEN1 (Presenilin 1), and PSEN2 (Presenilin 2). Mutations in these genes lead to an overproduction of toxic amyloid-beta peptides in the brain, which are linked to the development of Alzheimer’s.
While deterministic genes provide a clear link between genetics and Alzheimer’s risk, they account for fewer than 1% of all Alzheimer’s cases. Hence, while their impact is significant for the families they touch, they aren’t the primary genetic factor influencing Alzheimer’s on a larger scale.
Risk Genes
Risk genes increase the probability of developing a disease but do not guarantee it. For Alzheimer’s, the primary risk gene is APOE-e4. Everyone inherits one copy of the APOE gene from each parent, and there are several possible forms (or alleles) of this gene, including APOE-e2, APOE-e3, and APOE-e4. Out of these, APOE-e4 is the one with the most significant risk factor.
Having one copy of the APOE-e4 allele can double or triple an individual’s risk for Alzheimer’s. Having two copies (one from each parent) can increase the risk by up to twelve times. However, it’s essential to understand that not everyone with the APOE-e4 gene develops Alzheimer’s, and not everyone with Alzheimer’s has the APOE-e4 gene. This suggests that other factors, genetic and otherwise, also play a role in the disease’s onset.
The Genetic Landscape of Alzheimer’s: Beyond the Well-Known Players
While the likes of APP, PSEN1, PSEN2, and APOE-e4 dominate discussions about the genetic basis of Alzheimer’s, the genetic landscape is far more vast and intricate. With advances in genome sequencing technologies, researchers have been able to probe deeper into our DNA, leading to the discovery of numerous other genes that might have subtler, yet significant roles in influencing AD risk.
For instance, genes like TREM2 and CD33 have garnered attention in recent years. Mutations in the TREM2 gene, which plays a role in the immune response of the brain, have been associated with a several-fold increase in the risk of Alzheimer’s. CD33, another gene implicated in the brain’s immune function, has been shown to influence the clearance of amyloid-beta plaques—a hallmark of the disease.
Such findings hint at the intricate tapestry of genetic interactions at play. It’s not just about one or two key genes, but rather an orchestra of genetic elements working in tandem, sometimes harmoniously and at other times in discord, leading to the manifestation of the disease.
Looking Beyond Genes: The Epigenetic Perspective
Epigenetics, the study of changes in gene activity without altering the underlying DNA sequence, offers another dimension to our understanding. Epigenetic changes can be influenced by factors like diet, exposure to toxins, and even stress. These changes can turn genes on or off, affecting the production of proteins pivotal to Alzheimer’s.
There’s emerging evidence that epigenetic modifications, particularly DNA methylation, might play a role in Alzheimer’s. Understanding these epigenetic shifts and how they interact with genetic risk factors could pave the way for new therapeutic strategies and early interventions.
Environmental Factors and Lifestyle
While genetics plays a substantial role, it’s only one piece of the puzzle. Numerous studies have highlighted the influence of environmental factors and lifestyle choices in modulating Alzheimer’s risk.
For instance, cardiovascular risk factors, such as high blood pressure, diabetes, and high cholesterol, have been associated with an increased risk of Alzheimer’s. This implies that maintaining heart health could be crucial in reducing Alzheimer’s risk.
Moreover, there’s a growing body of evidence suggesting that brain-healthy lifestyles, which include regular physical activity, a balanced diet, mental stimulation, and active social engagement, can help in delaying or preventing the onset of Alzheimer’s symptoms.
The Microbiome Connection: Gut Health and the Brain
One of the most revolutionary findings in recent years has been the discovery of the gut-brain axis—a bidirectional communication system between our digestive system and the brain. Our gut is home to trillions of microbes, collectively known as the microbiome. These microbes play a pivotal role in our overall health, and intriguingly, there’s growing evidence to suggest a link between the gut microbiome and Alzheimer’s Disease.
Certain bacterial strains, when overrepresented in the gut, produce toxins that can cross the blood-brain barrier and induce neuroinflammation, a precursor to neurodegenerative conditions like Alzheimer’s. Conversely, a healthy and diverse gut microbiome might have protective effects, potentially reducing the risk of AD or delaying its onset.
As researchers delve deeper into the microbiome connection, there’s hope that interventions targeting the gut, such as probiotics or dietary adjustments, might emerge as novel strategies to combat Alzheimer’s.
Brain Connectivity and Neural Plasticity
For a long time, Alzheimer’s was predominantly viewed through the lens of protein accumulations and neuron death. However, contemporary research is shifting the focus to how brain regions communicate and how this connectivity changes over time, especially in the context of Alzheimer’s.
Neural plasticity refers to the brain’s ability to reorganize and form new neural connections. In healthy individuals, this plasticity allows for learning, memory, and adaptation to new experiences. However, in Alzheimer’s, this plasticity is compromised. Brain scans of AD patients often show decreased connectivity between different brain regions, especially those vital for memory and cognition.
Enhancing neural plasticity and connectivity might, therefore, be a therapeutic target. Interventions like cognitive training, brain stimulation techniques, and even certain medications aim to harness this principle to slow down the progression of Alzheimer’s or improve cognitive function in patients.
The Way Forward: A Call to Personalized Medicine
The interplay between genetics, lifestyle, and environment underscores the need for a more personalized approach to Alzheimer’s. This might involve genetic testing to identify high-risk individuals, followed by targeted interventions, such as lifestyle adjustments, early treatments, or even participation in clinical trials.
Researchers are hopeful that a combination of genetic insights and advances in other fields will lead to more effective treatments and prevention strategies for Alzheimer’s in the near future.
A Tapestry of Factors
As we’ve seen, Alzheimer’s Disease is influenced by a tapestry of interconnected factors. While genetics undoubtedly plays a role in determining risk, it’s not the sole determiner. Lifestyle, environment, and even epigenetic changes all contribute to the complex interplay that dictates whether someone will develop the disease. It’s crucial, therefore, to adopt a holistic view of Alzheimer’s, recognizing the multifactorial nature of its onset and progression. Through such an understanding, we move closer to a future where Alzheimer’s can be effectively managed if not entirely prevented.
Also, Read The Following: GoGoGrandparent review